The gut is home to trillions of microorganisms, including bacteria, viruses, fungi, and other microbes. In individuals with IBS, there may be an imbalance in the composition of the gut microbiome, with changes in the balance of certain bacterial species compared to healthy individuals. Research suggests that alterations in the composition and diversity of the gut microbiome can contribute to the development and symptoms of IBS. Here are some lifestyle factors that may lead to dysbiosis.

The gut microbiome plays a vital role in training and modulating the immune system. The gut microbiome interacts with the immune system, influencing its activity and response. Imbalances and dysbiosis can lead to immune system dysregulation and chronic inflammation in the gut. This inflammation can contribute to the development and persistence of IBS symptoms.
The gut is home to trillions of microorganisms, including bacteria, viruses, fungi, and other microbes. In individuals with IBS, there may be an imbalance in the composition of the gut microbiome, with alterations in the relative abundance of certain bacterial species compared to healthy individuals:

Antibiotics are designed to kill harmful bacteria, but they can also disrupt the balance of beneficial bacteria in the gut. Prolonged or frequent use of antibiotics can lead to dysbiosis by reducing the diversity and abundance of beneficial microbes.
The foods we choose feed our gut microbiome. Variety is key! Choosing high processed foods, refined sugars, saturated fats, and low in fiber can negatively impact the gut microbiome. This lacks the nutrients and diversity necessary to support a healthy microbial community, leading to dysbiosis. Dysbiosis can lead to the worsening of IBS symptoms.

Life can sometimes be stressful. Having chronic or high levels of stress can influence the gut-brain axis and lead to negative changes in the gut microbiome. Stress can alter gut motility, increase intestinal permeability, and affect immune function, all of which can contribute to dysbiosis.
Certain infections, such as bacterial or parasitic infections, can disrupt the gut microbiome. The infection itself, as well as the immune response against it, can lead to imbalances in microbial populations.

Certain medications can disrupt the gut microbiome and create negative changes with prolonged use. Two common examples are
Proton pump inhibitors (PPIs)
non-steroidal anti-inflammatories (NSAIDS)
PPIs can influence the gut microbiome in the following way:
NSAIDS can influence the gut microbiome in the following way:
The gut microbiome composition can change with age. Older adults may experience a reduction in beneficial bacteria and an increase in potentially harmful microbes, contributing to dysbiosis.
Skin conditions such as acne, eczema, rosacea, dryness and aging can also be affected by dysbiosis in vour skin microbiome. Skin microbiome testing is also available.

Exposure to environmental toxins, pollutants There are various environmental toxins that have the potential to disrupt the gut microbiome and contribute to dysbiosis.
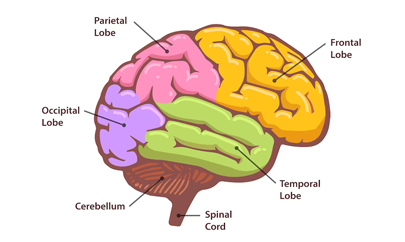
The gut-brain axis in IBS is like a messaging system that connects your gut and brain. It's a way for them to talk to each other and affect how you feel physically and emotionally. The Gut Brain consists of millions of nerve cells that communicate with the brain, influencing mood, stress, and pain perception, and the functioning of the digestive system. When you have IBS, this messaging system can get a bit out of sync, leading to stomach pain, bloating, and changes in bathroom habits. Stress and emotions can also make these symptoms worse. Understanding this connection can lead to better ways of managing and improving IBS symptoms. Its a bi-directional and biochemical link, which exists in all living organisms and not just in people with IBS.
The gut microbiome helps maintain the integrity of the intestinal barrier, which acts as a physical and functional barrier between the gut contents and the rest of the body. A disrupted gut microbiome can compromise the integrity of the intestinal lining, leading to increased permeability or "leaky gut." This allows substances, such as bacteria and toxins, to enter the bloodstream, triggering inflammation and IBS symptoms.
Studies have shown that individuals with IBS often exhibit alterations in the composition of their gut microbiome compared to healthy individuals. There may be an imbalance in the types and proportions of certain bacterial species in the gut, which can impact gut function and contribute to IBS symptoms. Reduced microbial diversity is commonly observed in individuals with IBS. A healthy gut microbiome is characterized by a rich and diverse community of microorganisms. Reduced diversity may lead to a less stable gut ecosystem and compromised functionality. The foods you eat can help to increase this diversity.

The gut microbiome plays a vital role in training and modulating the immune system. The gut microbiome interacts with the immune system, influencing its activity and response, Imbalances in the gut microbiome can lead to immune system dysregulation and chronic inflammation in the gut. This inflammation can contribute to the development and persistence of IBS symptoms.
The gut microbiome ferments undigested carbohydrates and fibers, producing gases like hydrogen, methane, and carbon dioxide. In individuals with IBS, the production and handling of these gases by the gut can contribute to bloating, abdominal pain, and changes in bowel movements. Our expert nutrition team will work with you to develop a customized meal plan that specific to your needs.


The gut microbiome has a role in the production of various neurotransmitters, including serotonin. Serotonin is a chemical messenger that helps regulate bowel movements and mood. Alterations in the gut microbiome can impact serotonin levels, potentially affecting gut motility and contributing to IBS symptoms.
The gut microbiome produces various metabolites through the breakdown of dietary components and other processes. These metabolites, such as short-chain fatty acids (SCFAs), can influence gut motility, immune function, and inflammation. Altered production of these metabolites in IBS may contribute to the development of symptoms.

Emerging research suggests that alterations in the gut microbiome may affect gut motility, intestinal barrier function, immune responses, and the communication between the gut and the brain, all of which can contribute to the symptoms of IBS. Dysbiosis has been associated with increased gut permeability, low-grade inflammation, and abnormal gut motility, all of which are believed to play a role in IBS. The great news the foods we eat, medications and our lifestyles can have a positive impact on the gut microbiome. We can see changes in our microbiome within days. During your journey with the BioGut Clinic we will complete 2 microbiome tests. One in the beginning and one near the end. At the BioGut Clinic we will explore probiotics, prebiotics, and dietary modifications to modulate the gut microbiome and alleviate IBS symptoms.